

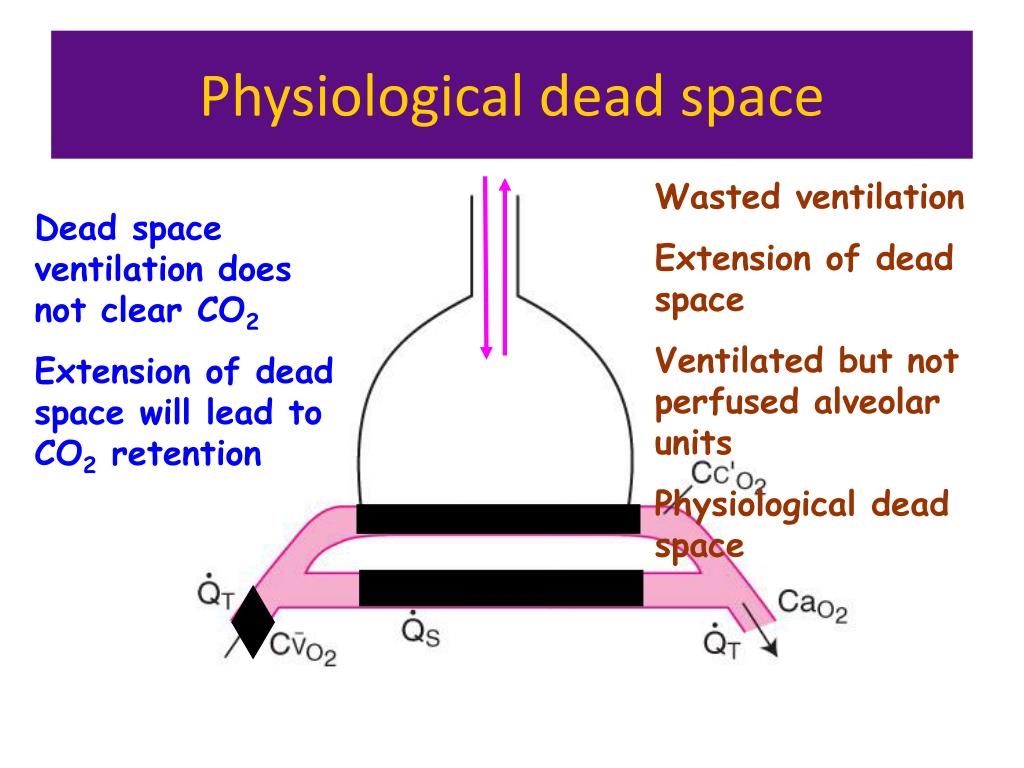
These factors are usually cited when explaining why a difficult to wean patient might be able to breathe unassisted through a tracheostomy tube but not through a translaryngeal ETT or, by inference, following extubation. The exact mechanism for improved clinical status remains ill-defined.īreathing humidified air through a tracheostomy tube differs from normal breathing via the intact upper airway primarily with respect to the volume of dead space and the impact of airway resistance. There is generally an improvement in clinical status following tracheostomy. Tracheostomy might determine whether a patient is ventilator dependent or successfully weaned. Endotracheal tubes (ETTs) increase dead space and elevate airway resistance, which could lead to excessive ventilatory support. This reduces the likelihood of tube obstruction by inspissated mucus, makes the patient more comfortable, requiring less sedation and reducing the likelihood of aspiration through improved glottic function.
Tracheostomy might facilitate weaning by reducing dead space and airway resistance, and by improving secretion clearance.
Tracheostomy is a surgical procedure routinely done in critically ill patients requiring prolonged mechanical ventilatory support.


 0 kommentar(er)
0 kommentar(er)
